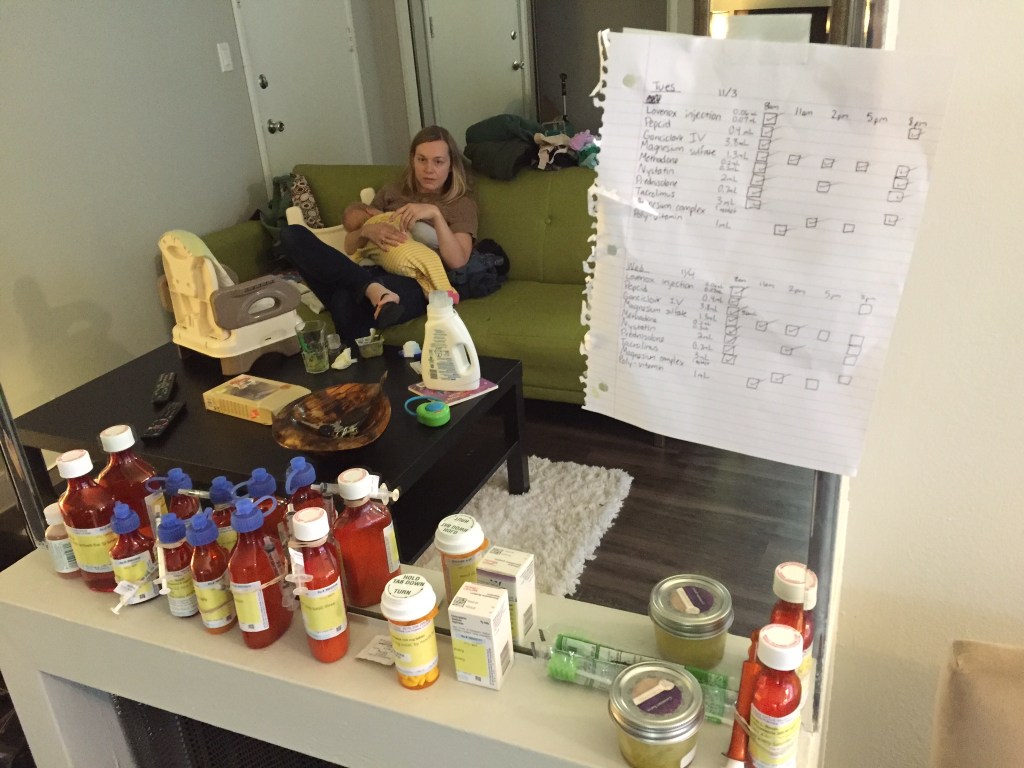
TPN is also called Total Perienteral Nutrition. It’s what they give patients who can not or should not eat by mouth. It basically is a recipe of all the necessary nutrition a person needs in order to get adequate vitamins, minerals, electrolytes, protein, fat, carbohydrates, etc. Since Norah was about 4 months old, the only weight she had put on was fluid buildup, called ascites. Once we got her on some very strong diuretics, she definitely shed the excess fluid but it also revealed to us just how small she actually was. After last week’s doctors appointment and UCLA the week before, it was decided that Norah begin getting TPN nutrition through her Broviac to help her body to absorb the necessary nutrients and gain weight/grow more appropriately. We were admitted on Wednesday, 8/26 to initiate TPN and also to possibly get a blood transfusion since her hemoglobin count was still quite low.

Today is Sunday and we are still in the hospital, so you can probable guess how well this hospital admission is going. We don’t have any idea how long we will be in this time as the initial estimate was about 3 days up to 7, but we are already on day 5 and her labs are still not where they want them and her belly has grown big with significant ascites (and quickly).
On Friday my head was not concentrating on timing and I realized too late that the nursing staff had forgotten to “wean” her from the TPN gradually so as not to put her at risk for a drop in blood sugar. Low and behold an hour and a half after ending the TPN, I picked her up and realized she was very shaky, almost as if she had a tremor. My gut reaction was that she had a blood sugar low but the doctors were called in and said that clinically she presented ok, but ordered a blood sugar test just in case. Whether it be mother’s intuition or not, I was right and her blood sugar had dropped to 53. I was able to breastfeed her and about a half hour after the initial blood sugar check, they did a follow-up check and it was 73, so in the safe zone for babies. Due to a drop in her sodium levels according to the labs that morning, they gave her a bag of saline to provide extra sodium to hold her over until her new mixture of TPN started around 9pm that night to run over 30 minutes. Being that she had to be hooked up again to the IV line and had just eaten, I figured it was a good time to shower and give myself a break. WRONG.

I was not in the room when they disconnected the saline bag and the nursing staff again made a major mistake in not flushing her Broviac line with heparin, putting her at major risk of blood clotting, which is life threatening since the Broviac basically goes into the main vein of her heart. The nurses quickly checked to make sure the line drew blood back and that there was no clots, and then lined the Broviac with heparin. I was so upset that I called one of our nurse representatives through the 3rd party company that works to coordinate care between home health, the hospital and our insurance. She called the case manager at the hospital and within about an hour the case manager and charge nurse came in to apologize for the missteps of the day. They told us that we would be reassigned a nurse for the remainder of the shift and that there was no excuse for the oversight and putting Norah at such a risk for complications.
Later that night Norah was fighting me on taking her medication and I had managed to get 4/5 oral syringes down when I must have put too much in her mouth, because she vomited some up. While I was initially upset because I wasn’t sure how much of the medication she had thrown up, I quickly realized that there was something different about this spit up. There were dark streaks in it. I immediately turned on the light to find that on her neck and on the front of her onesie there were dark brownish streaks of blood. This was a first and scared me half to death. I quickly hit the nurse call button, and after she had arrived she realized that the doctors needed to see Norah and the vomit as soon as possible. After some vague conversation, I still don’t understand how or why it happened, but ever since she has been given Zantac every 12 hours.
So to say that Friday was a bad day was a bit of an understatement. Thankfully my wonderful Aunt Cindy had flown in late Wednesday night and was there for Jason and I during the fiasco that was Friday (of course she had been there Thursday too but nothing crazy happened then, so we were able to just sit and visit). That night I was feeling more overwhelmed than usual and all I could do was hold my baby girl tight as we drifted off to sleep in hopes of a better day the next day.
Saturday was much better, but again she experienced a blood sugar crash about 1.5 hours after being weaned from the TPN. After talking with the doctors and nurses, it was decided to change both the rate of the TPN as well as extended the “wean” starting 2 hours before shutting it off (since it runs for 16 hours).

Then this morning I found out that now her sugar is stable, but her hemoglobin dropped again and now potassium did too. This resulted in a quick EKG to check to make sure the drop wasn’t affecting her heart. Seriously, this is turning into yet another rollercoaster ride, filled with snafus (mistakes) and I’m almost afraid to go home with her with so many things hanging in a delicate balance!